At Contemporary Jewish Museum’s Experience Leonard Cohen (1934-2016) exhibit, 18 men in their 60s and 70s sing from tracks of I’m Your Man – each recording in their own life-size monitor (modeling physical distancing during this pandemic!), and their synchronized voices form a cappella choir.
Well,
my friends are gone and my hair is grey
I
ache in the places where I used to play
And
I'm crazy for love but I'm not comin' on
I'm
just payin' my rent every day in the Tower of Song…
I
was born like this, I had no choice
I
was born with the gift of a golden voice…
--Leonard Cohen, “Tower of Song” from I’m Your Man (1988)
Like a choir, gerontology involves collaboration of many voices for a holistic approach to optimal aging.
Gerontology
is multidisciplinary in that it combines or integrates several separate areas
of study… fosters collaboration between physicians, nurses, biologists,
behavioral and social scientists, psychologists, social workers, economists,
policy experts, those who study the humanities and the arts, and many other
scholars and researchers in aging. Geriatrics, the branch of medical science
concerned with the prevention and treatment of diseases in older people, is a
part of the broader field of gerontology.
Gerontologists
improve the quality of life and promote the well-being of people as they age
through research, education, practice, and the application of interdisciplinary
knowledge of the aging process and aging populations.
--"What is gerontology?” Gerontological Society of America
Given the
dominance of the deficit-focused biomedical paradigm that views aging as a
disease for allopathic treatment, collaboration with other disciplines (shout
out to lawyers and occupational therapists!) allows for a more subjective
approach that includes voices of older adults based on their contextualized
lived experiences, strengths and what’s meaningful for them.
California Alliance for Retired Americans (CARA) hosted its 18th annual convention via Zoom. During online registration, participants selected just one of six workshop offerings (LTSS, Health Care, Affordable Housing, Climate Justice, Social Security, Nursing Home Reform), but technical difficulties with Zoom breakout rooms provided alternative opportunity to listen to all six workshop presentations with abbreviated Q&A. This workaround suited me because I wanted to learn from all six workshop presenters!
Long-Term Support & Services (LTSS)
Ramon Castellblanch, SFSU Professor Emeritus of Health Education (and a reader of my gerontology master’s thesis 😊), introduced LTSS for All! Lindsay Imai Hong, California Director of Hand in Hand Domestic Employers Network, said one in two Americans will need LTSS (broadly defined as assistance with activities of daily living, home modifications, durable medical equipment, etc.) in their lifetime. Existing public programs for financing LTSS are Medi-Cal In-Home Supportive Services (IHSS), Regional Centers for people with developmental disabilities, Veterans Affairs Aid & Attendance. Everyone else pays out of pocket, or relies on unpaid caregiving from family/friends/neighbors/charities.
Amanda Ream, Research Director at United Domestic Workers, representing 80,000 IHSS workers in California, presented The Care Agenda solution for universal LTSS!
Pres. Biden’s Build Back Better agenda includes “the most transformative investment in access to home care in 40 years, when these services were first authorized by Medicaid,” $150 billion (reduced from $400 billion in original proposal) to support people who need care (including 800,000 on waiting lists) and their paid caregivers.
Nursing
home reform
I
am petrified to get old. This disgraceful, broken system of senior living care
is something that we all need to care about. Because this is our future.—Kim Valentine,
elder abuse attorney, “State health department blasted over nursing home
oversight: Problems are staffing shortages, turnover, training and
pandemic pressures,” CalMatters (Oct. 6, 2021)
UCSF Nursing Professor Elizabeth Halifax said California nursing homes have had a humanitarian crisis with over 60,000 cases + 10,000 deaths among residents from COVID-19. She presented Nursing Home Reform policies to address problems of inadequate/unstable staffing; poor financial transparency and lack of accountability for use of public funds; lack of enforcement of existing regulations; state failure to vet owners/require licensing; failure to empower residents; inappropriate discharges; poor access to alternative/home care; outdated/unsafe nursing home environment.
Homeless advocacy
Janny Castillo, Director of
Community Outreach at St. Mary’s Center (its Geriatric Homeless Shelter was
profiled in The NYTimes) and Oakland Housing Authority Commissioner, presented on Housing for All, calling social justice
as wellness tool: fight to increase funding for safety net services, benefits
and affordable housing; protect poor people’s basic human rights by fighting
for decriminalization of those experiencing homelessness; advocate for better
mental health services; participate in peer-to-peer education and advocacy.
California Master Plan for Aging (MPA) San Francisco Regional Forum: Ending Homelessness Amongst Seniors and People with Disabilities (PWD) began with recorded intro by SF Mayor London Breed: “I was raised by my grandmother and she meant everything to me. Towards the end of her life, what mattered most was that she had the care and support she needed to continue to live with dignity. Everyone should be able to live and thrive without fear of ending up alone or on the street.” (Breed’s grandmother lived out her final years at Laguna Honda nursing home, notorious for patient abuse scandal uncovered in 2019.)
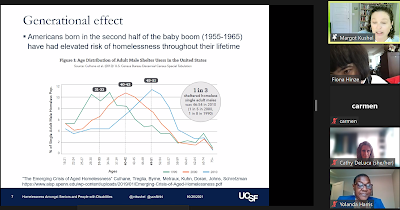
UCSF Benioff
Homelessness and Housing Initiative (BHHI) Director Margot Kushel, MD delivered keynote (almost same content as her 2019 Grand Rounds), followed by all-women panel! Most
importantly, this program included the voices of Del Seymour as panel moderator
and Yolanda Harris as panelist, who shared their own lived experiences with
homelessness.
“50 is the new 75” among homeless adults with overall poor functional status and geriatric conditions worse than those in the general population in their 70s and 80s. Dr. Kushel said the solution to homelessness is Housing First!
She provided examples of collaborations between aging and homeless services for low-income population:
· HomeSafe program involves Adult Protective Services (APS) to reduce eviction risks related to self-neglect. Some key findings from BHHI interim evaluation of HomeSafe pilot program are improved systems integration, limited usefulness of homeless risk assessment tool, and “some” clients helped to avoid homelessness.
·
PACE (Program of
All-Inclusive Care for Elderly) co-located with Permanent Supportive Housing (PSH).
· CAPABLE (Community Aging in Place—Advancing Better Living for Elders) for people located in PSH who are provided with a visiting nurse, occupational therapist, and handy person to modify home environment.
· Homebridge provides IHSS to PSH residents.
·
Project Roomkey provides
motel/hotel rooms to medically vulnerable homeless during COVID-19 pandemic (and prioritized older adults age 60+ with chronic
conditions).
COVID-19 vaccination rate among people experiencing homelessness was about 39% (much lower than 70% of San Franciscans) as of August, and access appeared to be a greater challenge than hesitancy.
Del Seymour said he was a 60-year-old disabled vet when Homeless Outreach Team worker got him off streets into Navigation Center, and then next day connected to Swords to Plowshares, which gave him keys to his 1st apartment; at that time, he was his own case manager hand-carrying paperwork between agencies working in silos because Veterans Affairs (VA) did not talk to Department of Public Health (DPH), which did not talk to Human Services Agency, which did not talk to…
·
Shireen
McSpadden, ED of SF Department of Homelessness & Supportive Housing (HSH), considered MPA Goal #1 as a call to action to fund housing options for older adults, also need for supports and universal design to
serve PWD, focus on preventing homelessness. Of the City’s existing 22,600
affordable housing units, over 13K or 58% occupied by seniors and PWD. She emphasized
need for partnerships between HSH and DAS (pilot enhanced IHSS in PSH), as well as DPH and
community-based organizations, to support people to age in place in PSH.
·
Kelly
Dearman, ED of SF Department of Disability & Aging Services (DAS), talked
about housing-related support services (rental subsidies, housing retention
support services in public housing, Home Safe-Phase 2); lowering barriers to
access like pilot to tailor co-located services to streamline IHSS eligibility.
·
Yolanda Harris, SF Housing Authority Commissioner, shared her own personal housing challenges
to help others navigate systems to access services.
·
Beth
Stokes, ED of Episcopal Community Services (and SFSU MSW alum), which manages
adult coordinated entry, said current challenge is focus on rehousing
shelter-in-place (SIP) hotel guests, and need to expand referral outside SIP pool to serve more for PSH available;
value of accessing services in neighborhood in which they’re from. She believes
we are capable of ending homelessness because pandemic showed how quickly we
can move to get people housed. She talked about PSH partnering/co-locating with
health care providers onsite, providing access to wellness program, recovery
and substance abuse services.
During
Q&A, I re-submitted question in chat that I emailed in advance that didn’t
get selected (“What metrics are used to evaluate effectiveness of contract
providers? What is being done to address high turnover among staff who serve
unhoused population to ensure these clients are not further traumatized when
people need more stable therapeutic relationships & ensure they do not fall
through the cracks?”), and surprised to receive chat comment from ol’ college
classmate (“Good point…it is difficult to recruit and retain staff in SF with
non-profit salaries. Staff cannot afford to live in the city”)!
Will higher
salaries address root causes of staff turnover? My HR Toolkit lists these reasons for high staff
turnover: overwhelming workloads, poor management, workplace bullying and toxic
culture, lack of opportunities for development, and better offers elsewhere.
Bullying is common in “caring” professions, and turnover makes sense for self-preservation: follow Robert I.
Sutton’s No A—hole Rule, and leave toxic work environment right away! While The Atlantic’s Derek Thompson considers quitting to be a sign of optimism (“We can do better!”), still waiting to see if employers get woke to
improve work culture. More power to The Revolt of the American Worker and The
Great Resignation!
Day after this program, the City’s HSH decided on extension to wind down SIP hotels through September 2022, to allow more time to relocate 1,400 SIP hotel guests (majority age 50+) to PSH. Cost of running single SIP hotel room (including meals, harm reduction supplies, health services, laundry and housekeeping services) estimated at $7K per month!
Gabor Mate’s Wisdom of Trauma (2021) documentary featured Downtown Streets Team (DST), a SF Bay Area nonprofit that claims to be “dedicated to ending homelessness” through “dignity of work” (unhoused “team members” start as “volunteers” to clean streets to “earn basic needs stipend” with potential to move up Team Lead-Manager hierarchy). Such an odd, creepy pick in light of news reports that DST executives involved in wage theft (settled), defamation, and allegations of sexual harassment and promoting drinking culture.
Dr. Mate followed up his documentary
with a series of conversations with trauma-informed providers. How Trauma
Literacy Can Transform Medicine was about mind-body-spirit connection: “If
you don’t know how to say no, your body will eventually say no for you…” Docs
talked about high suicide rate in their profession (higher than the military, and highest rate of any
profession), bullying in their medical training that resembles the
military. (Recognizing the harmful effects of bullying to patient care and team
dynamics, American Medical Association published Bullying in the
health care workplace: A guide to prevention & mitigation.)
“the story holds the key to what’s really going on, health is social well-being…” Patient’s life story provides context and allows patient to feel heard and seen.
Narrative-based medicine (NBM) came about in response to inadequacies of the biomedical model. According to George Zaharias, NBM is “a coming together of disparate schools of thought: the medical humanities (history, philosophy, ethics, literature, literary theory, the arts, and cultural studies); primary care and patient-centred care; biopsychosocial medicine and holistic care; and psychoanalysis and the work of Michael Balint.”
It is more important to
know what sort of person has a disease than to know what sort of disease a
person has.—Hippocrates, father of medicine
Chronic Pain and Trauma-Informed Healing discussion was multidisciplinary with MDs (Maté, Schubiner), life coaches (Ozanich, Rosen) and counselor (Wallin). “Wound is where the light enters the body”…reminded me of what Leonard Cohen sang in "Anthem"…
Experience Leonard Cohen included Judy Chicago’s paintings of his lyrics.
Ring the bells that
still can ring
Forget your perfect
offering
There is a crack, a
crack in everything
That's how the light
gets in
The birds they sang at
the break of day
"Start again",
I seem to hear them say
Don't dwell on what has
passed away
Or what is yet to be…
--Leonard Cohen, “Anthem” from The Future (1992)
As
gerontologist, enjoyed Experience Leonard Cohen exhibit and “10
Moments” mini-catalogue that mentioned his 2008-10 grand tour after a 15-year
break as Buddhist monk. Wish it explained septuagenarian Cohen got back on tour after he experienced elder financial abuse by his long-time manager, who embezzled his retirement savings. This could have been an opportunity to raise public awareness of elder abuse
and prevent such trauma from happening!
Elder Abuse Prevention
During COVID-19 pandemic, older adults have been targeted for financial scams. While perpetrators target vulnerable older adults (dependent due to cognitive/physical decline), behavioral scientists believe elder abuse prevention approaches could preemptively target populations who are cognitively vulnerable to deception and involve family caregivers in advance care planning like creating durable power of attorney.
Medical-Legal Partnership (MLP)
Bethany Hamilton, Co-Director of NCMLP at George Washington University, defined MLP as an intervention where legal and health care professionals collaborate to help patients resolve social, economic and environmental factors that contribute to health disparities and have a remedy in civil law. She said MLP is one of the only interventions that tackles individual needs and underlying policies: By detecting patterns in patients’ needs and using upstream strategies to target unhealthy policies, MLPs prevent future problems and advance health equity.
MLPs engage in these types of Patients to Policy projects:
1. Use data/stories to educate decision makers about the effects
of a policy
2. Meet with agencies to propose changes to application
requirements and procedures for benefits
3. Convene community stakeholders and decision makers
4. Challenge laws in courts!
NCMLP Toolkits:
· A planning, implementation, and practice guide for building and sustaining a health center-based MLP
· VA medical-legal partnership readiness guide
UCSF geriatrician Dr. Anne Fabiny presented on a “deeply engaged” MLP for seniors in SF VA health care system with UC Hastings School of Law. They began Transitions, Referral and Coordination (TRAC) team to care for older adults who are kept in the hospital for social, not medical, reasons because they don’t have a place to go and they end up living in the hospital more than 100 days, with the longest stay over two years!
Their strategies included
implementation of standardized process for reviewing need for probate
conservatorship for patients with dementia that ensures all other potential
options have been explored (veterans waiting for a conservator made up some of
the longest stays, now fewer patients referred for conservatorship); increased
use of Geriatrics Inpatient Consultation Service for capacity assessment; forum
for discussing challenging ethical issues and moral distress; and group
decision making about how best to engage family members in constructive problem
solving around discharge plans. (See Dr. Fabiny’s article, How an Interdisciplinary Care Team Reduces Prolonged Admissions Among Older Patients with Complex Needs.)
Lara Eilhardt, MLP Senior Attorney with Office of General Counsel at Department of VA, talked about legal needs as a social determinant of health because civil legal issues that can affect health and housing, if left unaddressed, can increase the risk of suicide. Based on CHALENG (Community Homelessness Assessment, Local Education and Networking Groups) survey, five of the top 10 unmet needs reported by homeless veterans require legal assistance: resolve child support, prevent evictions/foreclosures, restore driver’s license, address outstanding warrants/fines, and secure discharge upgrades. VA MLP services have improved veterans’ housing stability and mental health, and decreased their PTSD symptoms and reduced their substance use spending.
Check out Free Legal Clinics with VA Facilities.
Support Veterans Medical Legal Partnerships Act of 2021!
Pedestrian
safety
On sunny Saturday morning, advocacy groups Walk SF + Senior & Disability Action hosted walk audit for public to provide feedback to government agencies (SF Municipal Transportation Agency, SF Recreation & Parks), on Golden Gate Park (GGP) and proposed changes to car-free routes designed to promote equal access and improve traffic safety and GGP experience for all visitors.
Joined group with Walk SF Brian + SF Rec Brian to assess traffic along Fulton Street near 10th Avenue entrance to Golden Gate Park. Since this entrance has been closed to private cars during COVID-19 pandemic, there appears to be increased car traffic and occupied parking spaces outside entrance. But once inside refreshing GGP, less air + noise pollution from cars.
Adding more benches would make GGP more visitor friendly but alas the City has actually removed benches to discourage resting spots for unhoused people.
Here inside GGP’s car-free JFK Drive (where I paid attention to GGP shuttle for first time!), bicyclists did not observe STOP signs near pedestrian crossings. California’s Safety Stop Bill (AB 122) introduced to allow bicyclists to treat stop sign like yield sign, allowing them to proceed in intersections when clear and safe.
Before the pandemic, 75% of traffic used JFK Drive as a shortcut between places outside GGP--landing on the City's high-injury corridor with more than 100 injury collisions involving people walking/biking therein from 2015-2020. Since going car-free during the pandemic, zero collisions!
Plan for repaving this lot behind Music Concourse (which has its own 800-space underground garage that is pricey like Academy of Sciences admission tickets) to provide more parking spaces for people with disabilities.On busy Van Ness Ave. near SF City Hall, sign marks “someone died here”–11th pedestrian death this year, nearly half have been age 70+! Gov. Newsom vetoed Jaywalking Bill, which would have leveled playing field for pedestrians in car-centric roads.
Healthy aging
At virtual Hawaii Book & Music Festival, Healthy Aging program offered perspectives from University of Hawaii faculty from Geriatrics, Social Work, and Microbiology!
·
Geriatrics Professor at School
of Medicine (SOM) Kamal Masaki, MD, discussed geriatric approach to care (focus
on whole person, not organ systems, include physical, cognitive, psychologic,
social domains; enhance independence and quality of life; preventive care;
early rehab if possible; palliative care if necessary; interdisciplinary team
approach). Ideally, every older adult age 65+ would see a geriatrician,
except there is a shortage with only 7K geriatricians nationwide so now geriatricians
mostly care for very frail elderly. Shortage of geriatricians is less in
Hawaii, thanks to over 200 grads of UH geriatrics fellowship, many stay in Hawaii
and serve as consultants to primary care physicians; UH SOM also requires every
medical student to complete four weeks of geriatrics and palliative care
training. Hawaii has nation’s highest life expectancy due to Asian ethnic
groups (Chinese women live longest; Caucasians among lowest life expectancy). Women outlive men, but women age 70+ experience greater
physical disability and need for assistance with activities of daily living.
· Social Work Professor Emerita Colette Browne, DrPH, presented on older women and gender equity: advantages include longevity (nearly 70% of people age 85+ are women) and stronger social networks; disadvantages include lower income, health care and absence of LTSS. Despite improved gender parity in education, these gender inequities shape opportunities throughout their life course so women experience greater economic insecurity/risk of poverty in later life.
· Chancellor Emerita/Professor Virginia Hinshaw, PhD, presented on positive effects of aging, such as using both hemispheres of the brain (more compassion), decreased activity in amygdala (less response to fear, anger, hatred so become mellow and increasingly react to positive). She founded SOM Mini-Medical School on Healthy Aging in 2014, and now it’s available online.
Col-Labor-ation => retirement?
The latest issue of Public Policy & Aging Report focuses on Retirement Structures and Processes, noting a “decoupling of retirement and full labor-force departure” associated with decreasing financial security for many older workers, particularly since Great Recession of 2008. Redefining retirement today often includes some engagement in paid work, with opportunities in the gig economy and development of encore careers.
“My
new career is doing various stuff.
What’s needed to be done today? What can I learn today? What kind of
charges me up a little bit is being able to do something familiar and, at the same
time, having that opportunity to learn something new.”—Chris Francis, RV worker
in 400 sq. ft “house on wheels”, PBS Changing Work, Changing Workers
According to economist Teresa Ghilarducci, the future of work is connected to future of retirement income, and many older adults are working longer to supplement eroding pensions or declining Social Security benefits, while facing discrimination; she has called for creating Older Workers’ Bureau within U.S. Department of Labor!
Lawrence R. Samuel, author of Aging in America: A Cultural History (2018), views Boomers working as long as they can and aging in place (instead of fading into a life of leisure in a sunny retirement community) as a "wonderful development" to reintegrate older people back into the mainstream and possibly lessen ageism.
Musician-turned-social scientist Arthur C. Brooks noted that “having any job at all makes people happier” but “money as a career goal does not”; instead, he found job satisfaction comes from a good fit with your employer’s values and culture, and a sense of accomplishment.
…all over the world job satisfaction depends on a sense of accomplishment, recognition for a job well done, and work-life balance. Teamwork, too, has a strong influence in collectivist cultures, but less so in individualist ones. The late Harvard psychologist Richard Hackman found that job satisfaction was strongly, inversely tied to leader-centricity: In one of his studies, musicians who worked in symphony orchestras, where many conductors rule with an iron fist, were 21 percent less satisfied with their growth opportunities than players in leaderless string quartets.—Arthur C. Brooks, “The Secret to Happiness at Work,” The Atlantic (Sep. 2, 2021)
Very subjective! Brooks advises for real job satisfaction, we should pursue intrinsic goals like earned success (which employers can facilitate by giving “clear guidance and feedback, reward merit, and encourage their employers to develop new skills”) and service to others (sense of making the world a better place). For example, Brooks describes how his former student derived job satisfaction serving customers as waiter in Barcelona. (In contrast, Princeton grad Lillian Li did not derive job satisfaction from serving rude customers when she worked as waitress, but likely derived greater job satisfaction from writing about that experience in her novel, Number One Chinese Restaurant.)
Did Danish artist Jens Haaning derive job satisfaction from his “Take the Money and Run” delivery of blank canvases to Kunsten Museum of Modern Art as part of its Work It Out exhibit, in exchange for $84K?
Haaning insisted, “The work is that I
have taken their money.”
Kunsten CEO said, “This new work reminds us that we work for money.”
“Work”
is any job I do, paid or unpaid, that’s important to me. It’s anything I work
incredibly hard at, pour my heart and soul into — and anything that sits at the very core of
who I am and have always been.
I’m
a Mother, a Writer, a Musician, a Caregiver, an Athlete, and a Student.
And
work doesn’t define me — I define it.
I’m
a Caregiver for Seniors by day.
Although
I often feel like the clean version of a professional escort service for the
elderly — I love every minute of it…
Whatever
daily living activities my clients need help with, I always make sure my eyes
(and smile) are bright, my hair is pinned back, my scrubs are clean and crisp,
and I’m ready to show up for who and what they need me to be that day.
I
love helping people. I
love my Caregiving job because it doesn’t feel like work to me.
--Divina Grey, “Choose a Job You Love and You’ll Never Have to Work a Day in Your Life.” —Confucius. I know what I’m doing, even if you don’t think so. Medium (Aug. 14, 2021)
“Caregiver for Seniors” baffled me with her seemingly contradictory statements: concluding “I love my Caregiving job because it doesn’t feel like work to me” after previously defining “work is any job I do, paid or unpaid, that’s important to me.” And hope she is getting paid for job=work, for sake of funding her retirement! According to IRS, she is a “household employee” (employer controls work she does and how she does it) if she is paid more than $2,300 wages (2021), and both employer and employee obligated to pay Social Security + Medicare taxes.
National Retirement Security Month
Retirement security is a subject near and dear to me, as my pre-encore career was spent working in ERISA-covered retirement plans (investment management, trust administration, plan design and compliance, etc.). And I continue to live and breathe ERISA...
This month’s Women’s Institute for a Secure Retirement (WISER) conference looked at 25 Years of Improving Women’s Financial Security - Where We Stand: Possibilities & Progress!
Among the ways women can improve their long-term financial security are safeguarding one’s health and employability (keeping job skills up to date, networking, scoping out opportunities, etc.).
While other
countries have social safety net programs, women in USA have borne the brunt of job losses and caregiving burden during the pandemic. Since the beginning of 2020, 4 in 10
working women age 40-65 (and especially those providing care to others)
experienced job loss, reduced hours, furlough, temporary layoff, or reduced
wages --this translates to lower lifetime income, less savings, and reduced
Social Security benefits that undermine women’s retirement security.
In USA, retirement
security is “earned” during employment through payroll taxes (Social Security +
Medicare) and employer-sponsored tax-qualified plans (traditional defined
benefit pensions, defined contribution plans often with 401(k) salary deferral
feature).
Social Security Administration (SSA) announced that its annual cost-of-living adjustment (COLA) will increase to 5.9%, effective January 2022!
According to
Social Security and Medicare Board of Trustees’ 2021 annual reports:
· Social Security Trust Funds are projected to become depleted in 2034, one year earlier than projected last year, with 78% of benefits payable at that time.
· Medicare Part A (Hospital Insurance) trust fund is projected to run out of funds in 2026 (no change from last year’s report), and pay 91% of total scheduled benefits.
Data and projections were based on estimated effects of 2020 Recession (high unemployment) and COVID-19 pandemic on demographics (increases in deaths, decreases in births, and lower immigration rate): fewer people contributing to the funds, greater financial pressures. Call to action: Congress do something to address projected funding shortfall (e.g., increase amount of covered earnings subject to payroll tax)! To fix retirement income crisis, consider All Generations Plan (with caregivers’ credit for those who take time out of paid workforce to care for family members)!
2021-25 OAA State Plan on Aging, went into effect Oct. 1, 2021 (aka International Day of Older Persons!) —serving as a blueprint for CA’s #OAA network to build equitable, age-friendly communities through programs, partnerships, services, outreach efforts, and advocacy! Must read!