“…the space and time to be liked
exactly as you are feels like the most precious gift imaginable. The tranquil
rhythms of Won’t
You Be My Neighbor? remind us how simple the job of being a
good friend, a good parent, or a good citizen can be: You offer up your heart,
your patience, and your silence, and make some room for whatever your neighbor
might bring.” –- Heather Havrilesky, “Why Did We Ever Leave Mister Rogers’ Neighborhood?” New York Magazine (May
28, 2018)
When
older adults reside in age-segregated facilities, their world of connections
can get smaller… especially as peers die.
It’s hard for residents to share slow space with staff who are too busy
checking off their daily tasks.
Moving into assisted living/skilled nursing facilities really means joining
a disability community, as one 80-year-old resident told me that she felt she
had “aged ten years” because she was surrounded by so many residents with
multiple impairments, navigating the traffic jams of walkers/wheelchairs and especially
discouraged by a resident she befriended only to miss her due to her friend’s frequent
hospital stays. Residents also complain that
their children are “too selfish, self-absorbed, and busy with their own lives”
to contact them. Isolation and loneliness
can compound due to stigma of ageism and ableism, as I have encountered people outside of facilities who “do not wish to go there”
when I extend invitations to visit facilities.
I’ve been indulging in slow space …in life review with older adults, while incorporating Mister Rogers’ kindness, openness ("feelings are mention-able and manage-able") and unconditional positive regard (“Those who try to make you feel less than you are is the greatest evil” and “No person in the whole world is just like you, and I like you just the way you are”) … much needed, given longer and more complex lives. I also love the company of fellow introverts and models of civility and humility, PBS TV personality Fred Rogers and Supreme Court Justice Ruth Bader Ginsburg, who are subjects of my two favorite films this year, Won’t You Be My Neighbor? (95 minutes) and RBG (98 minutes, plus DVD extras). I admire RBG's gender equality advocacy and Olmstead decision; wish her complete recovery from lung surgery, as 85-year-old RBG expects to serve at least 5 more years on the Supreme Court!
I’ve been indulging in slow space …in life review with older adults, while incorporating Mister Rogers’ kindness, openness ("feelings are mention-able and manage-able") and unconditional positive regard (“Those who try to make you feel less than you are is the greatest evil” and “No person in the whole world is just like you, and I like you just the way you are”) … much needed, given longer and more complex lives. I also love the company of fellow introverts and models of civility and humility, PBS TV personality Fred Rogers and Supreme Court Justice Ruth Bader Ginsburg, who are subjects of my two favorite films this year, Won’t You Be My Neighbor? (95 minutes) and RBG (98 minutes, plus DVD extras). I admire RBG's gender equality advocacy and Olmstead decision; wish her complete recovery from lung surgery, as 85-year-old RBG expects to serve at least 5 more years on the Supreme Court!
Last
month, I managed to be a shut-in for a week to avoid outside air pollution from
the deadly Camp Fire (160 miles northwest of San Francisco). Even after the rains washed out the smokey
air, my allergies were severe enough that one facility resident told me that my
sniffling made her “nervous” and then suggested that I get a nose operation,
like she did, to clear my nasal passages.
Like Rudolph the Red-Nosed Reindeer, I did not get a nose job! Instead, I ended up taking antihistamines (children’s
dosage) for the first time in my life …
One
side effect of taking antihistamines is drowsiness, which is safer experienced
as a shut-in, especially avoiding traffic during winter holiday season. Also perfect for winter with longer periods
of darkness, I welcomed slowing down and sleep, particularly sleeping on the side,
which may be necessary to clean the brain of toxins. Researchers are studying the theory that sleep is necessary to clean the brain
of toxins, as this failure may lead to build-up of damaged proteins in the
brain that are associated with loss of brain cells in conditions such as
Alzheimer’s and Parkinson’s diseases.
Anyway,
as a sleepy shut-in, I stayed wide awake watching Miri Navasky’s Frontline
documentary, Living Old: The Modern Realities of Aging in America (2006), featuring
the old-old (age 85+), our fastest growing segment of the population, who often
have chronic conditions that require long-term care—60% of people who live past 85 will go
into a nursing home, and if they stay past 6 months, they may never leave. Documentary was made 12 years ago, but relevant take-aways:
· “When you're young, you want to live forever, ...but
many people don't want to live forever when they're old,” said William Coch, MD,
family practitioner in a rural New York community with a large older adult
population.
· “Someone
with three or more daughters or daughters-in-law has a better-than-even chance
of not ending up in a nursing home or institution,” according to Leon Kass, MD, Chair of
President’s Council on Bioethics which issued the landmark report, Taking Care: Ethical Caregiving in Our Aging Society (September 2005).
· David
Muller, MD, co-founder of Mount Sinai’s Visiting Doctors, made a house call to retired
physician Henry Janowitz, a widower with two daughters who live too far away to
be involved in his daily care, so he spends $150,000 a year (over $187,000
adjusted for inflation in 2018) for 24-hour help to remain at home! (Incidentally,
as Chief of Gastroenterology at Mount Sinai, Dr. Janowitz trained over 100
gastroenterologists, so he was able to boast that he could get sick in any
major town in the U.S., as long as it is a digestive problem, and be treated by
one of his students!)
To
age in place when you require long-term care, you need social capital (ready,
willing and able family members nearby) and/or financial capital (to pay the cost of care). Then when you move to assisted living or skilled nursing facility, it still
pays to have social capital for monitoring care (get chummy with your local long-term care ombudsman!) and providing companionship.
Filmmaker
Miri Navasky dedicated the documentary to her grandmother, Estelle Strongin
(1911-2006), who was featured as a 94-year-old stockbroker, working every day until she died
of heart failure three months after filming. May her memory be a blessing.
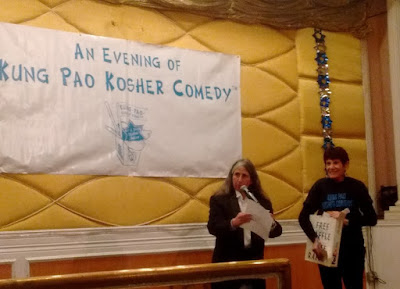
On
a cheerier note, I volunteered at the 26th annual
Kung Pao Kosher Comedy (KPKC), which sold-out all 6 shows (370 seats each)
during its 3-night run at New Asia Restaurant. (Mixed feelings about City of San Francisco’s plan to convert Chinatown’s largest banquet hall into affordable housing.) KPKC founder Lisa Geduldig and Volunteer Coordinator Dana Miller started the show
with raffle drawings.
Set
American-Chinese menu featured 6 courses (on rectangular table for volunteers
v. round tables for ticketed guests): Lisa G’s
Intergalactically-Famous Kosher (blessed by very reform rabbi) Walnut Prawns,
Kung Pao Chicken, Grandma Lillie’s Braised Tofu and Broccoli in Garlic Sauce,
Mixed Vegetable Chow Mein a la Boca Raton, Barbra Streisand’s Famous Green
Beans in Hoisin Sauce, Arline Geduldig’s World-Renowned Sweet & Sour Rock
Cod Filet) plus Steamed White Rice and Fortune
Cookies with Yiddish proverbs. Volunteering at KPKC has been my tradition since 2015 when Legal Assistance to the Elderly was a beneficiary, as ticket sales cover Charity + Chinese Food + Comedy!
Lisa
talked about starting KPKC at age 31 with a sold-out dinner show at 6 pm, next
year she added cocktail show at 9:30 pm, but now shows start an hour earlier so
the late show is now 8:30 pm. Noticed Lisa’s
trademark gray streak of hair framing her face now blends in with the rest of
her graying hair, so not sure about status of her film project, Is That Natural or Did You Dye It? Seque into Lisa’s more amusing
observations about the aging experience:
· forgetting
so she has breadcrumbs all over her home to help find her way
· finding
herself eligible for senior discounts when she turned age 55, though Ross Dress
for Less prematurely applied 10% senior discount when she was only 54.5 years
old
· thinking
it was Take Your Daughter to Work Day when she went in for a medical procedure
to see someone who could be her daughter treating her
· finally
pot is legal, but instead of getting high, she uses it to treat back pain (according to The New York Times’ Older Americans are flocking to medical marijuana, 33 states and the District of
Columbia have legalized medical marijuana, along with 10 states that also have
legalized recreational use)
Lisa’s 33-minute documentary, Esther and Me (2010), about
her friendship with octogenerian Esther Weintraub, former model and stand-up/sit-down comic resident at Jewish
Home of San Francisco, is now available for viewing online at http://www.cultureunplugged.com/storyteller/Lisa_Geduldig#/myFilms
Joseph Nguyen was born to a Vietnamese father and a Jewish mother who set-up a one-stop shop
where they filed nails and taxes! He wondered why people are proud just because
they are born with a race or place—“like, instead of being proud to be Korean,
it would be more impressive born a turtle and then you become Korean.”
When
Carol Leifer took the stage, she announced her age 62 to applause. She compared her old-timey name like Carol to
today’s popular names like Hannah, Zelda and Sophie—“sounding like an entry
list to Ellis Island all over.” Then she
told how she got into trouble with another old-timey name like Richard, which
is nicknamed “Dick,” but someone accused her of calling him “a dick.” She thought WikiLeaks was the name of a new
pad. Carol does not workout because her
philosophy is no pain, no pain.
Carol
is author of When You Lie About Your Age,
the Terrorists Win (2010), which is best read in her Long Island accent. The title of her book comes from realizing
that lying about her age was a no-go if she couldn’t share her greatest memory
to date happened when she saw the Beatles in a live concert at Shea Stadium in
the summer of 1966; invariably, people would ask, “How old are you?” In “Shea Stadium
and Its Effect on the Aging Process,” Carol reasoned, “when you deny your age,
you deny yourself … be who you are—memories and all.” She gloats over the realization that aging is
the great equalizer (or “old age is the revenge of the ugly ones”), so pretty girls who relied on their looks are “seriously having a hard time
now… When you don’t turn heads anymore and yours still just bobbles? Kinda
sucks, when you made sure to hit all those beauty appointments, but never once stopped
at a library. Geez, having a conversation is hard!”
Well, I never relied on my looks and libraries are my favorite hangout! I love the San Francisco Main Library's current exhibit, Visual Poetry: A Lyrical Twist. While I missed the opening event last month while homebound, SF Public Library recorded the event, which included readings by 85-year-old poet Jack Hirschman: “One day I’m gonna give up writing and just paint! … I’m gonna give up sitting and just breathe! I’m gonna give up breathing and just die! I’m gonna give up dying and just love! I’m gonna give up loving and just write!"
Well, I never relied on my looks and libraries are my favorite hangout! I love the San Francisco Main Library's current exhibit, Visual Poetry: A Lyrical Twist. While I missed the opening event last month while homebound, SF Public Library recorded the event, which included readings by 85-year-old poet Jack Hirschman: “One day I’m gonna give up writing and just paint! … I’m gonna give up sitting and just breathe! I’m gonna give up breathing and just die! I’m gonna give up dying and just love! I’m gonna give up loving and just write!"