·
In
USA, 1 in 7 people is a caregiver and more than 2/3 of people will need assistance
with daily tasks as they age.
·
In
USA, more than 53 million family caregivers provide approximately $470 billion
in unpaid support annually for their loved ones to be able to live in their
communities.
·
Family
caregivers often provide support without a formal assessment of their needs or
of the person receiving support; learn “on the job,” taking on complex medical,
administrative and care coordination activities.
·
Lost
income due to family caregiving is estimated at $522 billion each year.
Rosalynn Carter Institute for Caregivers’ Working While Caring: A National Survey of Caregiver Stress in the U.S. Workforce (Sep. 28, 2021) found that 1 in 5 full-time workers care for a family member with a serious illness/disability; nearly 20% of them quit a job to care for a relative, while 44% switched to part-time work. Rosalynn Carter has advocated for establishment of a new Office of Caregiver Health, within the U.S. Department of Health & Human Services, intended to improve coordination within the bureaucracy.
My
Administration is committed to strengthening American families and easing the
burdens of caregiving. That is why my American
Rescue Plan provided an additional $145 million in funding for the National
Family Caregiver Support Program,…also provided States with additional Medicaid
funding to strengthen and enhance their home- and community-based services
(HCBS) program. My Administration’s Build
Back Better agenda will build on this down payment by continuing to invest
in the caregiving infrastructure for HCBS and increasing pay and benefits to
address the direct care workforce crisis.
I will also fight to expand paid family and medical leave
nationwide. Each of these elements is
critical to better supporting family caregivers.
--Joseph R. Biden, Jr., A Proclamation on National Family Caregivers Month (Oct. 29, 2021)
It takes a
village + infrastructure, like job-protected leave and healthcare coverage, to
support family care partners.
· Effective Jan. 1, 2022, California Family Rights Act (AB 1033) expanded to grant eligible employees up to 12 weeks of job-protected leave to care for parent-in-law with a serious medical condition.
· Effective Jan. 1, 2023, Parent Health Care Act (AB 570) will allow adult children to add their parents/step parents (who are not eligible for Medicare) as dependents to their individual health insurance coverage.
https://twitter.com/CaregiverAction/status/1457888929127014402
This year’s NFCM theme is #CaregiverAnd, which encourages family caregivers to “celebrate the passions and interests that enrich their lives.”
During the COVID-19 pandemic lockdowns, many family caregivers were on their own without the usual respite supports from other relatives/neighbors/friends (as people formed their own pods/bubbles) and formal supports like home health/adult day centers/congregate care settings. Compared to non-caregivers during this pandemic, research found that family caregivers experienced higher rates of anxiety, depression and disturbed sleep; and reported less social interaction, more worries about finances and food, even after controlling for income and employment. Caregivers who fared the worst were female, young, lower-income, and providing care for people with cognitive disabilities (dementia) or behavioral/emotional problems.
According to UCLA study, Who Is Caring for the Caregivers? The Financial, Physical, and Mental Health Costs of Caregiving in California (Nov. 29, 2021):
·
In
2020, 1 in 4 California caregivers provided 20+ hours of care to a family
member/friend in a typical week, yet only 1 in 11 received payment for any of
the hours spent providing care
·
Majority
of caregivers in California are women (57.7%), middle age or ages 26-64 (67.5%)
and provide care to mainly older adults ages 65+(64.7%).
·
Nearly
half (44.4%) of California’s estimated 6.7 million adult caregivers reported
experiencing some level of financial stress in 2020 due to their role.
·
About
1 in 5 (20.9%) caregivers reported that caring for their relative/friend was
somewhat to extremely financially stressful.
·
1
in 7 caregivers (13.5%) reported a physical or mental health problem within the
past 12 months due to caregiving.
Aging boomers in later life have fewer family members to rely on for caregiving (due to never married, divorce, no kids, etc.). (China has recognized tradition of family caregivers, and “Confronted By Aging Population China Allows Couples To Have Three Children.”)
“I’m a single woman, so I say mom has me, but I don’t have a me.”—Lily Liu, who took “gap year” from her job to set-up infrastructure of care for her mom, featured in AARP documentary, Caregiving: The Circle of Love (2016)
(See Mission Local’s “For Mao survivors, the pandemic has been a cakewalk.” In 2015, Administration for Community Living awarded its first grant to develop “person-centered, trauma-informed” care for Holocaust survivors.)
Patti Davis wrote her handbook + memoir, Floating in the Deep End: How Caregivers Can See Beyond Alzheimer’s (2021), based on her caregiver support group, Beyond Alzheimer’s (started in 2011) and caring for her father Ronald Reagan who died in 2004. After her attempt to license Beyond Alzheimer's into “AA of caregiver support” fell through, she decided to write her book to share lessons, like addressing grief (“you’re well-served to inhabit and surrender to grief early on…grief is not biodegradable, it will wait and come find you…”), looking beyond disease to essence of person (“Alzheimer’s is stripping away of façade… my father was sweet, gentle person so it was easier”), educating about disease and acceptance to take on challenges like taking away car keys (avoid 86-year-old George Weller’s 20-second drive through farmer’s market in Santa Monica killing 10 people, and injuring many others.) She broadly viewed a caregiver as someone who shows up to provide support; her father received homecare from paid caregivers when he was “bedridden” during last three years of his 10-year illness.
“Kupuna edge”
“When you’re a caregiver … you’re the nurse, you’re the physician, you’re the lawyer, you’re the chauffeur, you’re the accountant. You play all of these different roles that most people go to school and get a degree for, and you are expected as the caregiver to become all of that overnight and as the disease progresses.”— Poki‘i Balaz, geriatric NP, “Our Kūpuna, Our Kuleana: Senior Care Crisis in Hawaiʻi,” Hawai’i Business (Feb. 4, 2020)
Growing up with kupuna (grandparents) in the same
household, family caregiving was reciprocal: my grandparents cared for me and
my siblings (while my parents worked outside of our home) until we became more
independent, and then we reciprocated as my grandparents with dementia became
more dependent on us for activities of daily living. This caregiver experience
was more like something we grew into as needs arose, rather than “overnight.”
And I suppose it helped that my grandparents had more than a single caregiver
playing different roles, and benefited from many family caregivers with
specialized roles including physician (though trained in OB-GYN; my cousin
didn’t become a geriatrician until after grandparents died), lawyer,
accountant, and we were all (non-degreed, but licensed) chauffeurs!
Last month, Hawaii Business magazine covered the role
of kupuna in caring for grand keiki in a series of articles about
Hawaii’s so-called kupuna edge:
· "Grandparents Help Hawai‘i Parents Get the Job Done: Grandmothers and grandfathers are storytellers, sources of wisdom, keepers of family legacies and teachers. But perhaps their most important role in Hawai‘i is to help working parents raise their keiki.”
· "Do’s and Don’ts of Using Grandparents for Child Care: Lessons learned from both grandparents and parents about navigating these relationships.”
· "Grandparents Are Great, But They Can’t Solve All of Hawai‘i’s Child Care Needs: Hawai‘i’s high cost of living often drives the need for grandparent-provided child care. But many grandparents can’t provide care because they are still working or live on the Mainland. Here’s what else is needed.” This article noted that grandparents who are the primary caregivers for their grandchildren tend to experience worse physical and mental health than those who provide occasional or no child care at all.
Kupuna might wish to exchange worse health for a stipend while serving in foster grandparent program and more low wage opportunities await them in proposed Caring Corps for older adults in charge of universal early childhood education?!
This month, the Advisory Council to Support Grandparents Raising Grandchildren (SGRC) released its Initial Report to Congress. Highlights:
· In USA, 2.7 million children are being
raised in the homes of grandparents.
· The child welfare system increasingly
relies on kin or grandfamilies to provide care for children, yet they are less
likely than non-related foster families to receive needed supports and
services.
This report also
provides recommendations that will inform development of the National Family
Caregiving Strategy.
As COVID-19
pandemic seemed to accelerate hospital discharge preference of patients to go
home rather than receive rehabilitation care from a skilled nursing facility
(SNF), some exciting Home- and Community-Based Services (HCBS) policy proposals:
· Choose Home Care Act of 2021 (S.2562/H.R. 5541) would increase access to health services at home by giving eligible Medicare beneficiaries the option to choose home-based extended care as an alternative to SNF care after being discharged from the hospital.
· Justice in Aging is advocating for change in federal Medicaid law to apply retroactive coverage of HCBS services after hospital discharge, just as Medicaid allows services to be covered up to 3 months for SNF.
Advance care planning
Geriatricians
are expert at managing syndromes that are associated with age (e.g., dementia)…
are good at deprescribing, looking at list of medications and possibility of
interactions…eliminating what’s not necessary… really useful if multiple
chronic illnesses… key to good care as we get older is constant, ongoing
communication with your doctor… about what you want, how aggressive you want,
that trade-off between things that might possibly prolong life versus
side-effects and quality of life.
--Jay Luxenberg, MD, On Lok Chief Medical Officer, “Do We Need New Doctors As We Age?” Not Born Yesterday podcast (Oct. 15, 2021)
UCSF geriatrician Dr. Anna Chodos presented on Advance Care Planning (ACP): how to make decisions based on context (emotions, needs, resources), personality, values, and experiences.
ACP includes medical and financial/legal considerations.
Wonder how many people attended this webinar? I asked all 4 questions! Answers:·
Even if elder orphan is
unable to name a surrogate, it is appropriate to document that person’s
preferences—even if “terrible system” for people who are not going to have an
advocate, POLST may or may not be useful.
· “Many of us deal with people who are really complex and seem to have a lot of wishes for what life is like now that don’t match up with what are some stated long-term goals like living forever, getting better…it’s a process we continue to revisit…most people do not like thinking about the hard stuff…Most people don’t get the point, they don’t understand what the heck we’re asking them to do…completing advance directive takes at least a half hour, if not an hour.”
· “Assuming they have a program where you can live forever,…what most religions promise people. No, I haven’t started referring people to Jehovah’s Witness programs, but I hope that was like a cheeky question…they’re plenty of religions that have very specific requirements for how people get healthcare.”
According to AARP, Hawaii has 157,000 family caregivers providing $2.1 billion value of u(n)paid care! AARP HI Pre-Crisis Planning for Dementia featured elder law attorney Laurie Adamshick, who shared her family caregiving experience.
For solo agers (“elder orphan” without family caregiver), she advised hiring a professional fiduciary.
Chinese American Coalition for Compassionate Care (CACCC) and AACI hosted Chinese American Cultural Challenges at End of Life (EOL) presented by Esther Luo, MD, Kaiser Permanente palliative care specialist. According to Pew Research, Asians are the fastest growing racial/ethnic group in USA, and Chinese are the largest Asian origin group making up 24% of this group.
According to California Health Care Foundation’s Help Wanted: Californians’ Views and Experiences of Serious Illness and End-of-Life Care
(2019), majority of Californians at EOL do not want to “burden” family, want
to die at home, prefer “natural death” and do not want to suffer pain.
Compared to whites, Chinese
Americans receive more aggressive EOL care including invasive mechanical ventilation when hospitalized and deaths in ICU so
fewer die at home.
Few Chinese Americans enroll in hospice due to cultural challenges, including finding providers with cultural sensitivity (honor family-based v. individual decision-making) and language fluency. About 25% of Chinese Americans live in traditional multigenerational household; modern Chinese family structure is more like the family depicted in The Farewell (2019) film: adult children live separately from aging parents, varying acculturation (immigrant with limited English so gaps in communication with USA-born children/grandchildren), working adult children may have limited time for direct care, so more common to hire or place elder in care home.
Traditional filial duties might include nondisclosure to protect psychological well-being of elderly parent; advocate for aggressive treatment to prolong life; pressure to perform duties to avoid disapproval of community (save “face”); provision of food at EOL as cultural obligation to demonstrate love and care.
“New” approach to filial piety involves ACP with parents initiating discussion and decision-making in context of not being burden to family, and reframing love/care by honoring elders’ wishes.
Good death is part of 5 blessings, along with
love of virtue, longevity, wealth, health. To traditional Chinese, components
of good death are defined by one’s accomplishments of familial responsibility;
“natural death” in old age; minimal suffering and free from pain; and maintaining
good family relationships.
Dr. Luo recommended indirect communication preferred
when discussing EOL: use another person’s EOL experience; frame discussion as
standard question and part of routine
care; acknowledge cultural taboos and ask for permission (e.g., some may fear
invoking “bad luck” if they discuss death, or talking about death might invite
death to come sooner); use provider’s own experience as example.
Last month, I completed mandatory First Aid/CPR/AED training. During COVID-19 pandemic to prevent contamination, rescuers place material over the victim’s mouth and nose. This mannequin did not look like Resusci Anne.
During COVID-19 pandemic, call 911 and stick to compression-only CPR: check for response, check for breathing (look; careful about exposure if you listen and feel), then start chest compressions 100-120 beats per minute to the rhythm of BeeGees’ Stayin’ Alive! Use AED defibrillator.
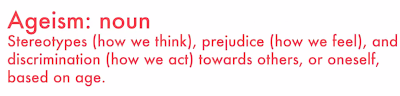
Ageism in healthcare
Kaiser Health News’ Navigating Aging columnist Judy Graham moderated stimulating 90-minute panel discussion, Confronting Ageism in Healthcare: A Conversation for Patients, Caregivers and Clinicians. What we can do:
· Louise Aronson, MD, UCSF geriatrician and author of Elderhood: suggested how to communicate with provider to get your needs met—e.g., “I feel that I’m not getting attention my symptoms warrant (use “I” statement), and I came to you because of your reputation as a good doctor” (compliment!). And she incited us to “make a ton of noise and don’t shut up until things change…that’s how other social change movements succeed, own it, be noisy. Let’s do it!” She added Essential Caregiver Bill (HR 3733) in Zoom chat box.
· Michael Wasserman, MD, geriatrician and immediate past president of California Association of Long-Term Care Medicine (CALTCM): encouraged us to “speak truth to power”; called out federal government spending $10 billion a year subsidizing graduate medical education, but failing to train doctors to care for Medicare beneficiaries; the failure to develop policies focused on older adults due to the lack of geriatric expertise among policymakers (notably, failure of Biden administration to appoint gerontology expert to COVID-19 task force)—“honestly, the federal government didn’t listen, and now we have over half a million deaths amongst older adults from COVID and close to 200,000 of them from nursing homes…honestly, the policymakers don’t seem to care.” (The lack of gerontology expertise proved fatal in nursing homes that cut off family visits since March 2020 through Nov. 12, 2021 when finally CMS lifted visitor restrictions in nursing homes.)
·
Rebecca
Elon, MD, geriatrician and family caregiver (see “Aiding Her Dying Husband, a Geriatrician Learns the Emotional and Physical Toll of Caregiving”): recommended starting local and with
groups for a louder voice!
·
Javette
Orgain, MD, family physician and medical director for Longevity Health Plan of
Illinois: called for intergenerational living, closing technology gap, increased
funding of home-based care and improving nursing homes!
· Jesse Mauer, JD, Executive Director of Maine Council on Aging, which promotes Anti-Ageism Pledge: advocated to include age in every DEI (diversity, equity, inclusion) conversation to “help us move collectively together”! (Check out recorded 2021 Wisdom Summit: Embracing a New Normal, Bouncing Forward to Build an Age-Positive Maine.)
Despite anti-ageism
guide to language tip, “do not use ‘elderly’ as a reference to a group,”
transcript showed use of “elderly” in reference to a group almost
interchangeable with “older adults” in same sentence:
·
Dr.
Orgain said she “began care for older adults prior to becoming a physician, so
I had some experience there that fostered my love for the care of the elderly.”
·
Judy
Graham asked Dr. Orgain about “the lack of resources and what that says about
how we approach our elderly population and what it means for those older
adults.”
Maine’s
Anti-Ageism Pledge includes “call attention to ageist language,” which depends
foremost on what “the person wants to be described” as an equity consideration,
and otherwise “refer to people over
60 as older people instead of seniors or the elderly.”
[Similarly,
University of Iowa researchers Clarissa A. Shaw, PhD and Jean K. Gordon, PhD,
advocate for an individualized, person-centered approach to communication
accommodation based on person’s preferences and needs, not stereotypes of aging;
for example, not all older adults find “elderspeak” (which arises when caregivers
take on parental role) to be patronizing, particularly when it facilitates
comprehension (e.g., slow speech, simplified sentence, long pause, loud voice, repetition,
etc.). Otherwise, elderspeak is harmful!]
Judy Graham summarized efforts to address ageism in healthcare: remove old age as a cause and symptom of disease; identify ageist beliefs and language (Frameworks Institute); tackle ageism at grassroots level (Changing the Narrative); require geriatrics education for medical students; include older adults in clinical trials; bring in geriatrics expertise; build age-friendly health system.
Joined screening of 16-minute video premiere of Changing the Narrative’s Antidotes for Ageism: A Brief Guide to Creating Inclusive Care in an Ageist Society, followed by discussion with talking heads from video. Take-aways:
· Our age does not define us (so stop attributing everything to “growing older”); instead, age-inclusive healthcare starts with caring for people as individuals because “every person is living a unique human experience.”
·
“If you are receiving care: Talk to your
provider. Ask questions. Your goals shape the course of your healthcare.
Clarify what you value to avoid under- or over-treatment. Advocate beyond
conversations with healthcare providers.
Seek care providers that truly listen to you, and support your vision
for your health.” (Can this be done in typical 15- to 20-minute visit?!)
·
“If you are a healthcare professional:
Active listening and letting patients guide care.”
Geriatrician Jeff Wallace, MD, advised: “Get to know the patient, whether they’re age 20 or age 80, and get the background, and that’s the fun part in many ways, to learn about your patient to start…the therapeutic relationship with a patient starts with respect. You have to respect them, and they have to respect you…doctors should be interrupted more often…it’s okay to say, ‘let’s just timeout, and I really want you to focus on this.’”
Consultant Carolyn Love said she understood that doctors and nurses are medical experts, but patients are experts of their own body so providers need to listen.
Gilliane Lee, recent graduate of occupational therapy (OT), talked about shift to focus on safety as well as quality of life for older adults, and responded to following Q&A:
Q:
What are some things that can be done to encourage more people to work with
older adults?
A:
“Bring them to assisted living facilities (ALF) and getting that exposure so
that they can understand that there is such a need for providing care.”
Oy vey, will exposure to ALF for understanding “need for providing care” translate to encouraging more people to work with older adults? Possible to deter people from working in ALF setting like Brookdale, the nation’s largest senior living provider and target of federal lawsuit on behalf of 83 families alleging elder neglect and financial abuse, as well as lawsuit by California Attorney General?! As a graduate gerontology student, I watched Life and Death in Assisted Living (2013), PBS Frontline documentary that featured my instructor Pat McGinnis, founder and Executive Director of California Advocates for Nursing Home Reform; that horror show convinced me to stay away from for-profit ALF!
“Too
many assisted living centers, care centers, and nursing homes are places I
would never allow a loved one to enter. Most wouldn’t either if they knew what
the facilities were really like. However, families who schedule facility tours
and interviews when considering placing a parent or grandparent, do not see
that side…Families must learn to get behind the scenes in order to see the truth.”
--Linda L. Schlenker, OTR, author of Aging in America: A Wake-Up Call and
Call to Action for Seniors and Those Who Love and Serve Them (2008),
calling out non-profit Mayo Clinic and St. Anne’s Home, Little Sisters of the
Poor (SF) as exceptional
Been there,
done that with my own stint working in ALF (non-profit, of course)! People who
get behind the scenes by working in ALF see truth of “need for providing care”:
understaffing, lack of staff trained in gerontology and experienced in working
with older adults, low morale, high turnover, etc. Residents who wait too long
for assistance end up trying to manage on their own, resulting in falls,
bedsores, medication errors, other neglect.
Exposure to
older adults segregated in ALF seems to reinforce warehousing people based on old
age/disability. More encouraging to meet older people where they are in a
variety of settings, listen and let their complexity grow on you until you
decide this could be an interesting way to earn a living 😉!
Ageism in media
Ageism isn’t even recognized in Pew Research’s list of 15 biggest problems facing the nation; in contrast, racism and sexism make the list.
November 2021
issue of The Journal of Gerontology: Social Sciences featured several articles
about media coverage of aging and ageism.
In Aging Narratives Over 210 Years (1810-2019), Reuben Ng, PhD, found aging narratives
in newspapers, magazines and nonfiction books have become more “negative” over
210 years, from “uplifting narratives of heroism and kinship” in the 1800s to
“darker tones of illness, death, and burden” in the 1900s as older adults came to be viewed as dominant occupants of almshouses and described as deserted by their
children and too infirm to work. Contributing to this ageism were the
diminishing status of older adults, loss of warmth, loss of competence, social
ostracism, and medicalization of aging. Defying this trend was fiction, which
provided “positive” portrayals of older adults through romantic courtship and
war heroism.
In Ageism in COVID-Related Newspaper Coverage: The First Month of the Pandemic, researchers analyzed 287 articles concerning older adults and COVID-19, published between March 11 and April 10, 2020, in four major U.S. newspapers (USA Today, The NY Times, LA Times, The WaPo), the term “ageism” appeared only five times and only in The NY Times opinion pieces, suggesting that journalists were not calling out ageism.
This failure to call out or name ageism seems to normalize ageism so it’s not viewed as the problem it is with harmful impacts.
Journalists
continue to confuse assisted living and nursing home, needing to issue
corrections like “This story has been corrected to refer to Brookdale as an
assisted living and memory care center instead of a nursing home.” In “The Forgotten Nursing Home Tragedy” (NY Times,
Nov. 4, 2021), journalist stated “Nurses were routinely working at several
elder-care facilities at once”—more likely the reality is lower-paid certified nursing assistants (CNA) who have closer hands-on contact with residents (assisting
with toileting, bathing, dressing, feeding, etc.) work at multiple nursing homes? Important to understand differences: ALF v. SNF, CNA v. nurse.
Wish more journalists would follow reporter Laura Wenus’ advice to consult someone with expertise in the field because “elder care and nursing care is a complex industry” so it helps to turn to a second pair of eyes to ensure “using the right terms and describing the relevant systems correctly.”
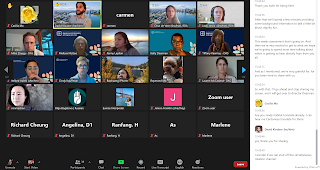
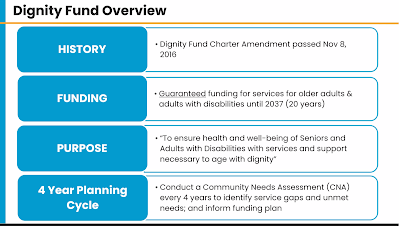
SF Dept. of Disability & Aging Services (DAS) hosted SF Dignity Fund Community Needs Forum (“What do older adults & adults with disabilities living in San Francisco need?). This took place on day after holiday weekend, 39 showed up on Zoom, mostly DAS staff; service providers who participated talked about workforce challenges like finding social workers who are Cantonese bilingual and who are familiar with African American culture.
I completed 36-item SF Dignity Fund Community Needs Assessment survey, commenting on need for gerontology training in workforce development to better serve diverse older adults, like designing a more age-friendly survey! Wonder how many older adults/people with disabilities had stamina to actually answer all survey items: e.g., 5-item Likert scales for #6 Please rate your agreement with the following (19) statements about your needs; #17 Please rate your agreement with the following (15) statements about any barriers you have experienced when trying to participate in services. By the time I got to survey's demographic information section, I just wanted to get over ordeal so quickly selected "Decline to answer"!