·
for
men: button-down shirts and pants/slacks, covered shoes with socks
·
for
women: sleeveless dresses/blouses ok, dressy sandals/slides ok
Four days later, AAGP
sent a follow-up email apologizing for its error after members pointed out that
its recommended attire “was not in step with current customs …nor with
recommended practices regarding how to acknowledge, validate, and make welcome
individuals who are members of gender or sexual minorities.”
Day 1
Aside from this misstep,
AAGP 2018 appeared to live up to its theme, “Diversity & Inclusivity:
Achieving Excellence in Geriatric Mental Health.” Given geriatric workforce shortages and dry spell of new blockbuster
drugs, AAGP sessions covered social determinants of health, positive
psychiatry, wellness and recovery, use of community health workers, more
collaborative care, technology—less traditional psychiatry with its emphasis on
pathology.
Global
Brain Health Research: Collaborative Partnerships to Advance Care and Build
Research Capacity - Martha Sajatovic, MD (Case Western) and
discussant Vikram Patel, MD (Harvard) discussed power of low-cost
interventions such as embedding front-line community health workers in health
promotion activities in households to detect depression and medication
adherence for chronic conditions.
Origins,
Past, Present and Future of Geriatric Psychiatry -
Sandy Finkel, MD, had 10 years of practice as a
geriatric psychiatrist when he became the founder and first President of AAGP 40
years ago. In 1977, Sandy met Gene
Cohen, MD, founding Chief of Center on Aging at National Institute of Mental
Health (NIMH) about establishing and growing the
incipient medical specialty of geriatric psychiatry: Gene’s focus on research, education and
public policy; Sandy’s focus on establishing an organization that would serve
as home for geriatric psychiatrists. In
1978, Sandy founded AAGP by calling a meeting in a hotel suite in Atlanta;
within a month, 300 members joined after paying dues at $3 per membership.
In 1993, AAGP began publishing its monthly scientific peer-reviewed
journal, The American Journal of Geriatric Psychiatry, with Gene as editor.
In 1978, geriatric
patients were hospital patients with personality disorders, Holocaust
survivors, state hospital patients (mostly with schizophrenia),
African-Americans from Southern origins, homosexuals, people in “old folks
homes”, people with impotence (pre-Viagara).
Future geriatric patients might include opioid addicts, prisoners, war veterans,
indigent baby boomers, record numbers of unemployed due to changing technology. To serve diverse populations, clinicians need
familiarity with a broad range of topics (alternative medicine, nutrition, sleep,
sexuality, religion, ethics, technology).
Later, Sandy joined
a panel that included Elliott Stein, MD, Director of
Psychiatry at Jewish Home in San Francisco and past AAGP President. In 1979, Drs. Finkel and Stein published special treatment planning for elderly to integrate DSM-3 clinical criteria to
older adults.
Hula entertainment
during Opening Plenary
AAGP President and University of Hawaii Clinical Professor of Geriatric Medicine Ike Ahmed, MD, mentioned this year AAGP celebrates its 40th anniversary and merger
with Geriatric Mental Health Foundation into a single non-profit organization under 501(c)(3). AAGP
President-Elect Melinda Lantz, MD (Mount Sinai, New York) delivered Plenary Address focused on search
for empathy: patients are often wiser
and empathic than we are; we start out life with empathy, especially first year
medical students but then empathy declines in 3rd year when they
start wearing white coats; role models are best example, need to promote and
embrace diversity to enhance empathy; barriers to empathy in clinical practice
are technology (email, LCD screens) and multi-tasking to keep away distraction. Solution is communication, face-time, and elevate
empathy leaders.
Reception in Great Lawn
– live band, finger foods and sunset.
Day 2
Breakfast Symposium: LTC for Patients with Parkinson Disease Psychosis
(supported through unrestricted educational grant from biopharmaceutical
company).
Meet
Me Where I Am: Expanding the Reach of Mental Health Services with Home and
Community-Based Services - Older
adults with mental health issues are less likely than younger adults to present
for care in specialty mental health clinics, due to barriers such as stigma,
transportation, accessibility and motivation to engage. Yet the negative
effects of untreated mental health problems in later life call for the use of
alternative treatment models that meet older people where they are.
- Renee Pepin, PhD (Dartmouth) presented Tele-Visiting for Home-Delivered Meals Clients, or use of video technology to deliver psychosocial interventions to Meals on Wheels clients.
- Kimberly Van Orden, PhD (University of Rochester) presented Participation in The Senior Corps as Mental Health Promotion, targeting social isolation. According to the interpersonal theory of suicide, people die by suicide if there is both desire (thwarted belongingness, perceived burdensomeness) and capability. Increased social connections can lower risk for suicide by changing perception; her study looked at peer companionship through The Senior Corps, a low-cost intervention that was associated with reduced perceived burden, depression and anxiety.
- substitute for Jo Anne Sirey,
PhD, on SMART-MH: Reducing Depression and Suicide Risk by
Integrating Brief Therapy into Senior Centers of NYC, with outreach and service delivery (brief needs assessment using PHQ-9, GAD-7,
Suicide risk; referral; offer brief psychotherapy ENGAGE to adults with
significant depression or suicidal ideation) to meet needs of older adults
in aftermath of Superstorm Sandy.
- Discussant Martha Bruce, PhD (Dartmouth) showed prevalence of major depression and rates of antidepressant use among older adults across the continuum of care. She spoke of expanding intervention targets and strategies to address complex biopsychosocial needs and circumstances (translational science), and improving access for vulnerable older adults by taking advantage of existing service infrastructure and workforce for screening, assessment, intervention and referrals (implementation science). She reviewed Penchansky's and Thomas' 5 A's of Access to Care: Affordability, Availability, Accessibility, Accommodation; and Acceptability.
Plenary: Universal Mental
Health Coverage Realizing Aspiration of Sustainable Development Goals, Sociocultural
Determinants and Treatment of Mental Disorders - Vikram
Patel, MD, said he traveled 36 hours from New Delhi on his first trip to
Hawaii! He reviewed WHO Sustainable Development Goal 3 for health targets
(improve mental health and well-being, prevention and treatment of substance
abuse, achieve universal health coverage) and WHO mhGAP Intervention Guide Version 2.0 (2016) .
Vikram showed this “reality”
graph illustrating divide between low-middle income countries and high income
countries, in both mental health care spending and people diagnosed with
depression who receive treatment. The
majority do not access quality mental health care. The solution is not putting more money into
the problem, but innovating to
address barriers:
·
human
resource gap: Vikram, author of When There Is No Psychiatrist: A Mental Health Care Manual (2003), wants
to train members of communities (community health workers, paraprofessionals,
peers) to give mental health interventions, empowering ordinary people to care
for others; this task-shifting to low cost health workers would be
supervised by specialists to optimize efficiency.
·
treatment
gap: deliver at home; self-management; e.g., home care project for dementia
uses non-pharmacological intervention, preventing depression in late life (DIL)
uses lay health counselors.
·
credibility gap:
prioritize patient needs; care not contingent on diagnostic labels; engage with
personal and community resources; address social determinants by incorporating
social work elements with mental health interventions.
He called for a collaborative care model,
involving a case manager who coordinates patient care with primary care
provider team, psychiatric/behavioral and medical team to optimize quality.
Sociocultural
Perceptions of Normal Aging—A Review and Media Presentation - Discussant Francis G. Lu, MD (UC Davis) (cultural formulation) with Ali Ashgar Ali, MD (Houston)(perceptions of aging more positive in Asian cultures; characters defy stereotypes in The Best Exotic Marigold Hotel) and Kristin Jones, MD (Baylor)(social constructs influence opportunities of Sadie and Bessie in Having Our Say: The Delaney Sisters First 100 Years).
Early Investigator
Poster Session and Exhibit Hall Reception
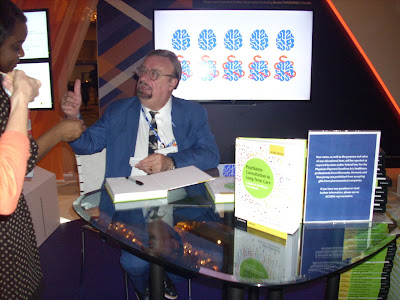
Author George T.
Grossberg, MD, autographed free (thanks to pharma company exhibitor) copies of his book, Psychiatric
Consultation in Long-Term Care (2010).
Embracing Hawaiian
Culture: Applying Traditional Hawaiian Values to Modern Ethical Decisions, presented by Joseph Dragonetti.
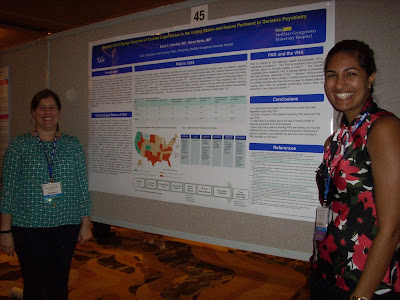
Physician Aid in Dying:
Overview of Current Legal Status in the U.S. and Issues Pertinent to Geriatric
Psychiatry, presented by Sarah Kleinfeld.
Social Work Shortage:
Can a Resource Packet Bridge the Gap in Care? presented by Chelsea Pluta.
Day 3
Positive Psychiatry in Geropsychiatric Clinical Practice: in
Schizophrenia, Cognitive disorders, and Affective disorders - Chair Dilip V. Jeste, MD of UCSD introduced
discussion on positive psychiatry, which is the “science and practice of psychiatry that seeks to understand and
promote well-being through assessments and interventions aimed at enhancing
positive psychosocial factors among people who have or are at high risk for
developing mental or physical illnesses.” Positive psychiatry views mental health and
illness as existing along a continuum (“wellness within illness” is possible). While traditional psychiatric treatments (psychotherapy,
psychopharmacology) focus on correcting deficits (checking off symptoms for
insurance claims), positive psychiatry focuses on building strengths to promote
wellness and recovery. In positive
psychiatry, there is partnership with patient who is empowered to actively
engage in intervention (“this is your care”).
Ellen E. Lee, MD, of UCSD presented on Childhood Adversity and Schizophrenia: Role of Resilience. Her research found that psychological resilience in adulthood appeared to counteract the negative effects of childhood adversity on mental and physical health in both adults with schizophrenia and non-psychiatric comparison adults.
People with schizophrenia experience earlier onset of aging-associated pathological changes (e.g., insulin resistance, immune activation, inflammatory syndrome, larger brain ventricles), as well as 2-12 times higher mortality, and 15- to 20-year shorter lifespan.
People with schizophrenia experience earlier onset of aging-associated pathological changes (e.g., insulin resistance, immune activation, inflammatory syndrome, larger brain ventricles), as well as 2-12 times higher mortality, and 15- to 20-year shorter lifespan.
Resilience is the
ability to adapt positively to, or to recover readily from, adversity; it is
associated with medically desirable behaviors (self-care, treatment and exercise
adherence), better health outcomes (emotional health and well-being, less pain,
better physical health) and greater longevity.
People in their 90s who endorsed higher
levels of resilience had 43% higher likelihood of living to 100 years.
Resilience-enhancing
interventions include Stress Management and Resilience Training (SMART based on
adaptation of attention and interpretation theory), Mindfulness-Based Stress
Reduction (MBSR based on meditation, mindfulness, guided imagery and hypnosis),
and novel biological interventions (training to modulate one’s own brain
activity with real-time MRI-based neuro-feedback).
Here are 10 steps to
Resilience, from Resilience: The Science of Mastering Life's Greatest
Challenges (2012) by
Steven Southwick and Dennis Charney:
1. Positive attitude (optimism)
2. Cognitive flexibility (reframe, assimilate,
accept, recover; failure is essential for growth)
3. Personal moral compass (set of core
beliefs)
4. Role model (imitation is powerful mode
of learning)
5. Face your fears (fear is normal,
facing fears can increase self-esteem)
6. Develop active coping skills
7. Establish and nurture supportive
social network (very few can “go it alone”, considerable emotional strength
accrues from close relationships)
8. Attend to physical well-being
(exercise)
9. Training (discipline and practice)
10.Recognize, utilize and foster your
strengths (engage character strengths to cope with stress)
1. Problem definition: reframe “a problem
well-stated is a problem half-solved”
2. Goal setting
3. Brain storming: break negative spiral
4. Considering pros and cons
5. Decision making
6. Action planning
7. Evaluation
Taya Varteresian, DO of Los Angeles, presented
on Complementary Alternative and Integrative Medicine (CAIM) & Whole
Medical Systems. At
$33.9 billion, CAIM accounts for about 1.5% of total health care expenditures,
and 11.2% of out-of-pocket health care expenditures in U.S. Mind-Body medicine, such as yoga, meditation
(Kirtan Kriya is user-friendly for older people), natural products and
supplements (adaptogens such as St. John’s wort, SAMe, melatonin, etc.), have
potential to enhance resilience to stress by rebalancing autonomic nervous
system (increasing parasympathetic and decreasing sympathetic output,
increasing GABA levels), decreasing inflammation, changing epigenetic and gene
expression, and by direct neuroplastic effects on the brain. She also discussed value of interdisciplinary
team (social workers, case managers, RNs, geriatricians, psychiatrists) and
benefits of geri-psychiatry home visits (removing stigma of visiting mental
health clinic, gaining knowledge of home environment).
Plenary: Cultural Neuroscience by Joan Chiao,
PhD read through power point presentation just under 30 minutes, followed by a
few questions and brief answers … then we were out early for beach time 😊.
Aging and Post-Intensive Care Syndrome (PICS): The Burden on Older ICU
Survivors and Their Families based on article
published in February 2018 issue of The
American Journal of Geriatric Psychiatry,
by Chair Sophia Wang, MD, and colleagues from Indiana
University—Babar Khan, MD, Noll Campbell, PharmD, and You Na P. Kheir, MD. Highlights:
·
More
than 50% of Intensive Care Unit (ICU) admissions are patients age 65+ and 70%
of them develop delirium. Due to rapid
improvements in ICU care, survivorship from critical illness is “now the
defining challenge of critical care medicine” as ICU survivors may develop
long-term cognitive, psychological and physical impairments from their critical
illness—aka PICS, which is more likely to affect
older adults.
·
Only
about 50% of all older adult ICU survivors have functional recovery after their
critical illness, with median recovery time of 3 months and increased need for
support outside the hospital. Higher
body mass index and functional self-efficacy associated with better post-ICU
recovery. Physical disability was significant
contributor to depression at 3 and 12 months after ICU hospitalization.
·
Risk
factors for ICU-acquired long-term cognitive impairment (LTCI) in older adults
include neurologic dysfunction, infection or severe sepsis, and acute
dialysis. Yet evidence does not strongly
support that older adults at higher risk than younger adults for LTCI.
·
Depression,
anxiety and post-traumatic stress disorder (PTSD) are mental health impairments
in PICS. However, patients who develop
critical illness may be more likely to have premorbid psychiatric illness,
compared with those hospitalized in general wards and the general population.
·
ICU-related
risk factors for PICS-Family impact include perception of patient being very
near death, unexpected/sudden patient illness, family members with greater
levels of anxiety and depression about ICU hospitalization, and poor
communication between family members and ICU physicians. Interventions for PICS-F include diaries and educational
materials; condolence letters written to family members may actually worsen
their depression and PTSD-related symptoms.
·
Indiana
University’s Critical Care Recovery Center, first dedicated post-ICU survivor
clinic in the U.S. created in 2011, uses innovative collaborative care model
(including family conference, recovery care coordinator follows to outpatient
setting) that has been shown to be successful in older adults with dementia and
late-life depression.
Improving Mental Health
Care Access, Engagement and Delivery among Diverse, Underserved Populations:
Collaborations from Geriatric Mental Health Services Research T32 Postdoctoral
Fellowship - Mentor
Steve Bartels, MD of Dartmouth noted that older adults
age 65+ with mental health or substance use disorder receive inadequate care:
only 10% receive any treatment, and
mere 1% receive specialty mental
health services.
Accurate
and effective implementation of research-based practices takes 17 years!
People with serious mental illness,
about 6% of the U.S. population, have one of the greatest health disparities of
any group, with a life expectancy up to 25 years less than the general
population from complications of unhealthy risk factors that may be preventable.
Fellows presented data on disparities in mental health care and then addressed
the diverse, complex mental health needs of older adults through adapting
evidence-based prevention and self-management programs to improve effectiveness
and uptake:
·
Chair
Daniel Jimenez, PhD (Miami) on Happy Older Latinos are Active (HOLA), multicomponent
health promotion intervention to prevent anxiety and depression in older Latinos.
·
Mijung
Park, PhD (UCSF) on Family-Centered Care for Older Adults with Multiple Chronic
Conditions (FACE): Adding family components
to Collaborative Care Model for Older Adults with depression and chronic
medical conditions.
·
Matthew
Lohman, PhD (SC) on Hospitalization Risk with Potentially Inappropriate Medications.
· Karen Whiteman Fortuna, PhD (Dartmouth) on PeerTECH: Peer-Delivered and Technology Assisted Psychiatric and Medical Illness Self-Management for Adults with Serious Mental Illness.
Improving Competency in the Care of the Older Transgender Patient: A Case Study with On Lok social worker Wing Yee Wong, MFT from San Francisco. I mentioned that I referred a homebound transgender woman client to On Lok, and then realized this client was the subject of her poster! Small world.
Day 4
AAGP Advocacy: Strengthening Our Mission in Geriatric Mental Health - Ilse Wiechers, MD, Chair of AAGP Public Policy Caucus, provided advocacy tips. Becky
Yowell, American Psychiatric Association (APA) Regulatory Policy Deputy Director, delivered Legislative and Regulatory Update:
·
Federal
legislative successes (Comprehensive Addiction and Recovery Act, 21st
Century Cures, Defeat of ACA Repeal/Replace Legislation); budget deal; Medicaid
work requirements (Section 1115 waivers); opioid epidemic (funding, legislation);
substance use disorder confidentiality (42 CFR Part 2 reform); Mental Health Parity;
telehealth/telepsychiatry (CHRONIC Act, CONNECT for Health Act, Veterans
E-Health and Telemedicine Support), workforce development (Resident Physician
Shortage Act).
·
State
legislative issues: scope of practice; network adequacy; mental health parity; Medicaid
(funding, expansion, physician reimbursement); medication access (prior
authorization, step therapy); access to telemedicine/telepsychiatry; state
opioid epidemic measures (PDMP reporting); inpatient/outpatient involuntary
treatment; criminal justice (“drug courts”, solitary confinement); maintenance
of certification; tort reform; state suicide prevention/anti-bullying
initiatives.
Cultural Competence in Palliative and End-of-Life Care: Understanding
Your Patient’s Context - Chair Greg Sullivan, MD provided introduction on History
of Cultural Competence in EOL Care (person-centered care, AAGP’s Best Practice Highlights for Treating Diverse Patient Populations) and Symptoms at EOL (meanings of pain).
Patricia W. Nishimoto,
DNS, self-described Iowa farm girl who moved to Hawaii to work as oncology nurse, presented on
The Magic of Expressive Arts in
Palliative Care and Cultural Complexities.
Her presentation, illustrated with photos of patients, asked us to
consider:
·
Cultural
curiosity approach when interacting with patients: listen with humility, ask respectfully
about their beliefs, and view world through their cultural lens.
·
Conflict
is more about emotions than factual misunderstandings.
·
Role
of family: who makes decisions? Who’s included in discussions? Is full disclosure
acceptable?
·
Verbal
communication: if insulted when offered interpreter, explain interpreter is for
medical, not language; do not ask, “do you understand?” instead ask them to
repeat information back to you.
·
“Difficult”
usually means there are unmet needs. Look
for red flags: repeat visits without resolution of problems; demanding; dependent;
manipulative; stubborn; nonadherent; power struggles; self-destructive
behaviors; focus on seemingly unrelated issues.
·
Self-reflection:
how you identify racially, ethnically, and culturally? When were you first
aware of your own culture? What is the first memory you have of someone dying
in your family? What were the rituals, practices or behaviors that your family
observed at that time? What aspects of your cultural background do you feel
strengthen your caring for dying patients and their families?
Matthew W. Warren, MD (Tampa) presented on End-of-Life Issues for
Non-religious Patients:
·
Informed
patients are less likely to receive invasive procedures or die in ICU
·
Existential
distress (mortality, freedom, meaninglessness, isolation)
·
Sigmund
Freud: death is the aim of all life; death cannot be feared since it has never
been experienced
·
Existential
psychotherapy: Choron’s 3 types of death fear (what comes after death, event of
dying, ceasing to be); competing death defenses (schizoid=independent of all
control, passive-dependent=give up all control); death as opportunity
(rearrange priorities, enhanced sense of living in present, deeper
communication with loved ones); awareness (ultimately no escape from death,
face life alone, ultimate responsibility for way one lives); activities that
provide sense of life purpose (altruism, dedication to cause, creativity,
hedonistic value, self-actualization, self-transcendence)
·
Atul
Gawande’s Being Mortal: Medicine and What Matters in the End (2014)
·
Irvin
Yalom’s Staring at the Sun: Overcoming
the Terror of Death (2009)
·
Approach:
start conversations using patient’s own words; clinician may ask, “are you at
peace?”; allow patient to retain sense of dignity (show interest, allow choice,
respect privacy); assess how much patient would like to know; engage in conversation
about hope (legacy potential); address patient’s preferred “place of death” (only
1 in 3 patients in U.S. die at home)
Kenneth M. Sakauye, MD,
presented on Cultural Competency in
Palliative Care about a mandatory month-long, pass-fail Geriatrics-Palliative
course at University of Tennessee. APA
Council on Aging has 3 cultural competency guides, updated about every 10 years:
·
APA Culture, Heritage
and Diversity in Older Adult Mental Health Care (expected
2018; Maria Llorente, Chair)
·
APA Ethnic Minority Elderly Curriculum
(2006; Ike Ahmed, Chair)
·
APA/AAGP Curriculum Resource Guide for Cultural Competence
(1997; Kenneth Sakauye, Chair)
Managing Behavioral Health Needs of Older Adults in the Emergency Department --
Laurel J. Bessey, MD (Madison) provided an
overview of substance use disorders (alcohol, illicit drug, opioids),
depression (affects 3-7% of older adults, 1/3 of older adults seen in ED screened
positive for depression) and suicidal ideation (older adults accounted for 16%
if all suicides, though only 12% of adult population), anxiety (most common
psychiatric symptom affect 15% in community populations) and panic in older
adults in ED.
Rebecca M. Radue, MD (Madison) provided an
overview of psychosis (most common etiologies are dementia and delirium), agitation
(common, life threatening emergency; non-pharmacologic interventions include
warm blanket, get down to patient’s level, provide nourishment, use calm voice
and short, simple phrases, validate). Management
principles call for trying non-pharmacologic strategies first; then if
pharmacologic strategies are needed, use lowest possible dose, consider black
box warnings and avoid benzos in delirium.
Discussant
Lisa Boyle, MD (Madison), asked Brent Lu, MD, about the situation in Hawaii, which he
described as challenging due to shortage of mental health services and geriatric
psychiatry beds for older adults, reluctance of long-term care facilities to
admit psychiatric patients, caregiver burnout, etc. – resulting in increased
reliance on emergency services often involving law enforcement.
Lisa noted to consider
context of local policies; for example, Wisconsin has restrictive involuntary mental
health statute that requires “treatable mental illness”—some interpret
Alzheimer’s as not treatable so no access, and people end up in jail due to misunderstanding
that no cure, but can treat to alleviate suffering; psychiatrists do not have
final say in emergency detention, but defer to county crisis worker and police.
Death Café + Dementia Care
People with mental
disabilities, including dementia, often get “stuck in place” or confined in
locked facilities and out-of-sight from the broader community. As a gerontologist, I have sought to gain
experience at each level in the continuum of care: aging in place, family care,
senior centers, adult day care centers, home care, retirement and independent
living communities, and assisted living.
As new staff in an assisted living community, I did a stint in “memory care”/locked facility floor (residents
with varying levels of memory loss mixed with other residents who were high
functioning but somehow determined to need higher level of care than assisted
living), which I found oppressive so immediately ended that not-to-be-repeated experience. Imagine if I had been a resident on that
floor, I’d be dead due to transfer trauma.
I suspect transfer trauma contributed to
my grandmother’s death shortly after she moved into a nursing home for dementia
care. Before my grandmother’s death, I never gave any serious thought to anything
beyond aging at home. After all, filial
piety was ingrained in my Chinese immigrant family so it was assumed family
members took care of one another at home.
In my previous career in banking, my high net worth clients could afford
live-in home care to support aging at home.
But people have always moved for mobility,
so Hawaii’s Brain Drain makes it harder for offspring living outside Hawaii to be
physically present to provide care to parents aging in Hawaii.
During my visit to Honolulu last fall, I attended a workshop taught by Dorothy Colby,
certified Positive Approach to Care trainer, but did not have time to tour the
memory care home where she is administrator.
In the AAGP 2018 Annual Meeting Schedule, I noticed Dorothy was
scheduled to present Challenging
Behaviors in Dementia Care: Recognizing Unmet Needs – A Positive Approach to
Care Seminar.
Honolulu is a small town as I
ended up meeting Dorothy when we both showed up at 11th Death Café Honolulu, organized by Leilani Maxera, whom I met during HPGS conference over three years ago.
At Death Café, participants drink tea, eat cake, and
discuss death with “aim to increase awareness of death to help people make the
most of their (finite) lives.”
As contribution to potluck, bought Leonard’s Bakery malasadas
coated in plain sugar, li hing mui and cinnamon.
Over two hours, we enjoyed potluck treats while covering a
broad range of topics from UH Willed Body Program, sea burials, Death Over Dinner, death doulas, hospice volunteering,…
reactions to facing death during false missile threat, Jewish death rituals, films about death, Philip Roth's
Patrimony, aid in dying, etc. Always good to know
options! Most attendees were women, who are leading movement to bring
back home funerals!
After reconnecting with Dorothy at Death
Café, I visited Hale Ku’ike for a morning tour with
Dorothy and Community Relations Director Scott Gardiner. There were 26 residents, mostly female, with
average age 91 years.
View of courtyard from inside common area
Namaste Care room
Sorting/folding laundry table
Access to outdoors with labradoodle named Pepper
Other home-like design features: human-scale,
picture windows that bring in natural sunlight, laminate flooring, memory boxes
outside room doors, greenery, spacious common area, etc. During morning tour, all residents
were congregated in common areas while resident room doors were left wide open
(no photos allowed). Monthly cost of private
room is $9,770, and semi-private room is $8,110. Instead of TV watching, daily schedule of
activities include:
Hale Ku’ike Nu’uanu Club
7:30 am BREAKFAST (protein, starch, fruit, skim milk,
fluids)
8:30 am Volunteers at Work and Gardening (includes sorting
activities and other meaningful “work”, taking care of outdoor planter boxes)
9:30 am Morning Greeting Songs (singing Star Spangled
Banner, Hawaii Ponoi, God Bless America to open up day)
9:35 am News and Views (current events, seasonal talk,
horoscopes, weather, etc.)
9:45 am Eldercise (exercises focusing on range of motion,
flexibility, mobility, strength and balance)
10:30 am Morning Garden Walk
10:45 am SIT & SIP (AM snack: fruit slices, water)
11 am Morning Surprise (changes daily: food trivia,
remanence time, armchair travel, special entertainment, etc.; Tuesdays Tai Chi
at 11:15 am)
12 noon LUNCH (meat, vegetable, soup, starch, fluids)
12:45 pm Games People Play (small group activities include
variety of cognitive exercises and table games; Mondays Song & Dance with
Nalani at 1:45 pm)
2 pm Fun & Games (physical activities focusing on fun
& fitness)
3 pm CHAT & CHEW (PM snack: fruit slices, water)
3:15 pm Afternoon Delight (group activities with
occasional holiday specific ones; 2nd, 3rd & 5th
Friday with Pastor Dan at 3:30 pm)
4:15 pm Brain Teasers or Music Moments (cognitive word
games, trivia, sing-a-longs)
4:45 pm Evening Garden Walk (outdoor walk before dinner to
stimulate senses)
5 pm DINNER (meat, vegetable, starch, skim milk, low-fat
dressing/butter, fluids)
6:30 pm Evening Cinema
BEDTIME SNACK (skim milk, water)
As an introvert, I need
quiet time to doodle which is best done in solitude and not group setting. For people who are religious minorities (e.g.,
Jehovah’s Witness or Jewish), participation in singing patriotic/nationalistic
songs, horoscopes, and holiday activities would be uncomfortable. In person-centered care, these preferences
should be respected.
Aging in place
According to AARP,
nearly 90% of adults age 65+ want to stay in their current home and community as they age, which is associated with maintaining independence, autonomy, and social
connections in their neighborhoods and community.
The benefits of a community of strong connections,
which require time to develop, come from the fact that it is rooted in place,
such that people have a relationship with a place they call home, which is
“integral to their identity and well-being, and to their cultural and political
values,” as noted by Naomi Schoenbaum, in “Stuck or Rooted? The Costs of Mobility and the Value
of Place,” Yale Law Journal (October
30, 2017).
However, many homes may not be designed to accommodate the needs of aging residents. During my visit, Honolulu Mayor Kirk Caldwell signed a moratorium on monster homes while Hawaii legislature considered mandating visitability standards on
publicly funded housing (SB 2594). Aiyah! Because my parents’ privately funded,
custom designed home includes many visitability features, such as wheelchair
accessibility, it is a spacious monster home intended for my parents to age in
place. My parents completed their
accessible home nearly 15 years ago—long before LineSync’s Wheel Pad came
into the picture.



























































Hawaii governor signs bill legalizing medical 'aid in dying'
ReplyDeleteThursday, April 5th 2018
By Jim Mendoza, Reporter
HONOLULU (HawaiiNewsNow) -
With the stroke of a pen Gov. David Ige erased 20 years of emotional debate Hawaii has held over medically assisted suicide.
Surrounded by lawmakers and supporters of the Our Care, Our Choice Act, Ige signed the bill into law.
"We have gotten to a point in our community that it does make sense to give the patient a choice to request the medication, obtain it and take it, or ultimately change their mind if they so choose to," he said.
Ige called it the logical next step for dying patients, giving them an option besides palliative care..
Hawaii is the seventh jurisdiction in the U.S. to legalize death with dignity.
Adult patients who are terminally ill have to meet strict guidelines to get the life-ending prescription medication.
Cancer sufferer John Radcliffe said it's important patients have that option.
"Every other living democratic governor also supports this merciful action to make dying less terrifying and far more peaceful for those up against a tortured passing," he said.
Opponents fear elderly and disabled people will be pressured to end their lives. They worry the law could encourage people with depression to consider suicide.
But supporters point to safeguards.
Someone who wants the medication must meet counseling requirements and be mentally competent. In addition, two doctors have to agree that the patent has less than six months to live.
Rep. Della Au Belatti authored and introduced the measure.
"It's a choice an individual can make so they can think about how they want to live the rest of their life," she said
"We know that our loved ones will eventually die but they don't need to suffer," Ige said.
The law takes effect January 1, 2019.
http://www.hawaiinewsnow.com/story/37890922/hawaii-governor-set-to-sign-medical-aid-in-dying-bill